While the French government has launched a general vaccination campaign (supported by the Institut National du Cancer) against HPV in French secondary schools, aimed at 5th graders, it is still estimated that almost 8 out of 10 people are exposed to Human Papilloma Virus (HPV) in the course of their lives. This high figure may reflect a lack of awareness on the subject…
What is HPV? What are its long-term health consequences? Why get vaccinated, and who is concerned?

How does the vaccination campaign work, and who is involved?
In order to reach an important milestone in cancer prevention, the government has decided to roll out a vast vaccination operation, from October 1, 2023, across the whole of France, with the support of the Regional Health Agencies, healthcare professionals, the rectorat and professionals from the educational community.
More concretely, from this date onwards, mobile teams of healthcare professionals from ARS-accredited vaccination centers, or from vaccination centers run by departmental councils that retain responsibility for organizing vaccinations, will travel to all secondary schools (public and private under contract) to provide vaccination sessions during school hours. These mobile teams can also be backed up by healthcare professionals (doctors, nurses, midwives or pharmacists), whether they are working, retired, salaried, unemployed, civil servants or students.
National education staff are also mobilized to provide information to parents and pupils, and to liaise with the health professionals who will be involved in the vaccination campaign. They will also be responsible for setting up the premises in the field to ensure smooth operation (confidential area, appropriate equipment, water point, etc.).
Mobile vaccination teams are responsible for ensuring compliance with the logistics chain for the vaccine, which is packaged in single-dose, ready-to-use doses. They are responsible for transporting the vaccines to the dose storage area in the school, and for returning unused doses to the vaccination centers.
How is the vaccine transported and stored?
If a vaccine is naturally stored in a refrigerator, what happens in the field during a vaccination campaign if such facilities are not readily available? The HPV vaccine must be kept continuously at temperatures between +2°C and +8°C, both during storage and transport (like any other vaccine, according to the WHO).
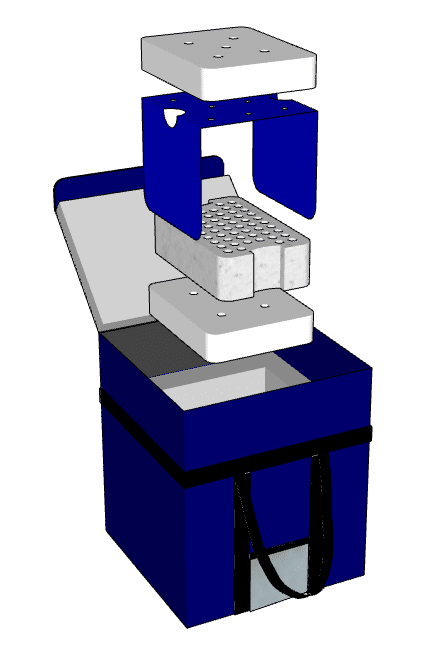
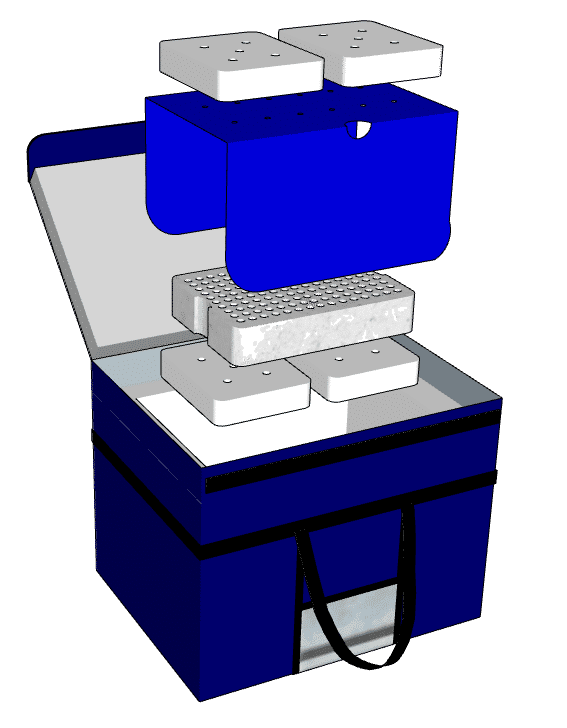
To support Regional Health Agencies and other healthcare professionals in this area, COLD AND CO has developed the MedicalCase, a professional passive-cooling medical cooler that guarantees temperature maintenance for heat-sensitive healthcare products, without the need for continuous energy input (such as electricity).
Thanks to the use of eutectic gels (previously frozen) inside the cooler, COLD AND CO’s MedicalCase is capable of maintaining a precise temperature for up to 72 hours (the number of gels determines this duration). A real asset when access to equipment delivering continuous active cooling is not possible or too costly.
Available in volumes ranging from 5 to 84 liters, the MedicalCase cooler for healthcare professionals is also ideal for transporting and storing other types of heat-sensitive healthcare products, such as blood derivatives, oncology products and biotechnology products.
To find out more :
What is the Papillomavirus and why get vaccinated?
More commonly known as papillomaviruses, Human Papilloma Virus (HPV) infections are common, widespread viruses – in fact, there are almost 200 types. Transmission and contamination occur almost exclusively through sexual contact. Once contracted, these infections can infect mucous membranes as well as the skin, and can be responsible for benign or malignant lesions. For the most part, HPV infections do not cause any lesions, and in 90% of cases, the infection clears up naturally within one or two years of contamination. This is known as a « transient » infection. In 10% of cases, however, the infection persists and can lead to lesions, mostly on the cervix. These lesions are called « precancerous » and can develop into cancer 10 to 15 years after their appearance.
Although transmission occurs through sexual contact, condoms do not provide 100% protection against HPV infection, as they do not cover the entire genital area. Only the vaccine protects against HPV (with efficacy close to 100% in a young population). Although not compulsory, vaccination is strongly recommended by the French National Authority for Health.
Who is affected by the vaccine and how does it work?
Even if HPV is most often associated with cervical cancer (and rightly so), we must not reduce it to this simple expression, and realize that HPV infections affect all populations, women and men alike. That’s why vaccination is recommended for « all girls AND boys aged 11 to 14 » (INCa). The vaccine is all the more effective as this population has not yet been exposed to the risks of HPV contamination. The current vaccination campaign (free of charge) in French secondary schools should therefore enable an increase in vaccination coverage, which is well below the target of 80% by 2030. It should be noted that, in addition to this campaign, which will protect up to 800,000 pupils a year, prescription AND vaccination can be carried out by nurses, midwives and pharmacists.
For young people aged 11 to 14, the vaccination schedule is based on 2 injections of vaccine, spaced 6 to 13 months apart. A second vaccination schedule, known as catch-up, involves 3 injections for previously unvaccinated 15-19 year-olds.
Today, 2 vaccines are available: a bivalent and a nonavalent. These vaccines are not interchangeable, which means that the booster dose must be administered with the same vaccine as the first dose.